Many people have a period of dementia before they die. Indeed, dementia has been identified as the leading cause of death in the UK. The diseases that cause dementia are often described as cruel: typically they slowly erode a person’s memories, knowledge, understanding, and eventually the ability to talk, walk and swallow. LSE Philosophy Professor Anna Mahtani spoke to three women whose life has been impacted by dementia in very different ways.
Who is caring for people with dementia and other illnesses? In many cases family members – partners, children and other relatives – take on this task. And the task is not shared equally across society: around two thirds of unpaid carers of people with dementia are women; female carers spend more hours on their care-giving role than male carers; and they are 2.5 times more likely to live with the person that they care for. Many of these carers are juggling other responsibilities such as work and childcare: between the ages of 45 and 54, one in five women will provide unpaid care to an older friend or relative (see here for references to the stats).
What is the impact on these carers? Though they are many in number, we don’t often hear their views, and they have been described as invisible members of our society. I spoke to three women who wanted their voices to be heard.
No choice
Maria used to work in television documentaries, but now manages the care for her elderly parents who have a rota of 10 people looking after them. Her dad has had dementia for 36 years, diagnosed when he was 50 and caused by alcoholism. She describes the experience of caring for her parents as “horrible”, but doesn’t usually feel able to say so: “You’re supposed to go around saying that they are marvellous for their age and that you want the best for them, and you do, but you also don’t want twenty years of caring for somebody severely mentally and physically disabled who hasn’t got a clue who you are”.
Life with Maria’s parents can be difficult and chaotic. At one point her mum was happy to let her dad starve to death, and wouldn’t let anyone else interfere, so Maria had to contact social services and ask them to intervene. Maria saved her father’s life that day and doesn’t regret it, but says “a couple of years on I thought, what did I do that for? Just so he could go round with his offensive delusions costing everyone else an arm and a leg?”. She says “I honestly think that there is something wrong with a society where a lot of people are reduced to wishing other people dead for their own sake, as well as because it is ruining the family’s life”.
Eldercare is importantly different from childcare, as Maria points out. Firstly, the need for very involved care can last much longer: “I’m horrified that having required 10-15 years of intensive care as a child, I’m now faced with possibly double that for people who are seriously mentally and physically disabled”. Secondly, while childcare ends (or diminishes) when the child becomes an adult, the endpoint of eldercare is death: as Maria says: “It’s an obscene reversal of what care should be”. Thirdly, while having a child is often a choice, that’s not always the case with eldercare, and Maria’s experience is that this caring role has been forced on her. And finally while those doing childcare are partially supported in society, those doing eldercare are not – neither financially, nor with a free equivalent of the daily care that school provides.
Being a support-human
Ali works full-time and has a teenager, but also spends around fourteen hours per week caring for her parents. Her mum had a stroke several years ago and is paralysed on one side and unable to speak. Ali feels like she is the “support-human” for everyone in her life: “Everyone wants more, and your own time just gets smaller and smaller and smaller. Middle-aged women are invisible – you’re just there to skivvy for everybody.”
Ali loves her mum, and hopes that once she’s gone she’ll be able to remember how she was. But right now, the person that she’s caring for does not seem like her mum – though “there’s bits of her that are still there”. The great unsayable truth is that sometimes Ali wishes that her parents were dead. She says “Four years ago it would never have occurred to me that I would wish they were dead. But now my dad’s miserable, my mum’s miserable, and I’m miserable. And every hour that I spend over there is an hour that I’m not spending with my daughter. There are no winners in this scenario and we’re all just having to keep going”.
I asked Ali what she would change, and one theme that emerged was around treatment. She says “I don’t think it’s about euthanasia, but rather about withdrawal of treatment by the family or the patient or the doctor. Our society’s got a fear of death, and it’s seen as a failure if the doctor does not keep people alive. When people are grieving they want to blame other people – but doctors shouldn’t be facing criticism when they have a very elderly patient with lots of co-morbidities, who is clearly never going to get better, and they decide to make them comfortable and not prolong their life. Medicine should be less about can we? – because the answer is almost always yes we can – and more about should we?”
The death you would choose
Finally I talked to Sofia who is now retired, but worked for many years first as a midwife, then as Matron of a dementia care home, and then as a carer for people with dementia in their own homes. She found it very rewarding but challenging. She emphasised that there are many different kinds of dementia, and that even individuals with the same diagnosis will present differently. Dementia is not just memory loss, but involves all systems of the body – and there is no effective treatment. Sofia’s experience has taught her that the best approach is to agree with everything that a person with dementia says, even if it is false. Otherwise, the experience of constantly being told that you are wrong, and having to be told – as if for the first time – that loved ones have long-since died, is a frightening and distressing experience. She says that people with dementia are “not in this world”.
Sofia has had her own experience of caring for an aunt with dementia. She talked about the time it took, the endless phone calls, and the juggling of these caring tasks with her job. She ended up taking Valium, needing therapy, and then time off work with stress. In her professional caring role, Sofia has also witnessed many family members (“it was generally daughters”) going through a similar experience. She says: “Caring for elderly parents with dementia or terminal illness is the next most important feminist issue which we need to get to grips with. There are plenty of younger feminists who are not aware of this, and they need to have their consciousnesses raised by older feminists. And the government is doing nothing to support carers or pay them. Carer’s allowance of £71 per week is a joke”.
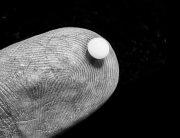
Sofia also has views on life-prolonging treatments. “I have nursed patients where some of the carers did not understand that giving antibiotics was prolonging the agony. I have nursed patients who have been tube fed for literally years! We have arrived at this point because people cannot accept death. They cannot even say ‘dead’, but say ‘passed’ ‘passed over’, ‘passed away’ to sanitise and sweeten it. People die. They are born then they die. My own mother died of cancer, and we nursed her at home, just for three weeks. We specified no antibiotics, but wanted good pain relief, so mum had heroin and morphine. It is the sort of death that all would choose.”
Hearing carers’ voices
Talking to these three women gave me a glimpse of the suffering that is happening around the UK – affecting both people who need care and the people that provide it. And this is borne out in large-scale studies: see for example this recent report which finds that 89% of dementia carers have reached crisis point at least once, and that one in three carers described their emotional health as either bad (27%) or very bad (7%). And it’s not just a UK problem: the number of people globally living with dementia is set to almost double every 20 years, and much of the increase will be in developing countries. If you want to have a big effect on wellbeing – perhaps you’re an effective altruist interested in human wellbeing specifically – then this seems like a good place to focus.
What can be done? The women I interviewed put forward a number of changes that they would like to see, and these included making care homes not-for-profit organisations, ensuring fair pay for professional carers, and protecting the rights of informal carers. But a consistent theme was around re-thinking life-prolonging treatment in cases of severe dementia and other terminal illness in the elderly. This re-thinking could come from three different angles: we might encourage individuals to make an advanced directive so that they can choose their own limits; we might seek to remove some of the disincentives on medical staff to switch to palliative care; and we might try to make it easier for relatives to ask for life-prolonging treatment to cease in cases where it seems to be in no-one’s best interests.
For this last shift, I think that changing the way that we talk can help. We talk as though any recovery is always positive. If you hear that a friend’s elderly relative has rallied, you might automatically interpret that as entirely good news. But the women I talked to made clear that this is not always the case. It’s taboo to say so, but sometimes carers are hoping for a decline which will eventually end the misery for all.[1] When something is taboo, it’s hard to even think it clearly, and – I’d imagine – very hard to say it to a doctor asking what treatment you’d like your relative to have. One step we can take, then, is to make this easier to say. We can bring to light and affirm these carers’ entirely legitimate feelings, and start talking about what we really want the end of a life to look like.
By Anna Mahtani
Anna Mahtani is a Professor at LSE Philosophy. She works on the philosophy of language, along with decision theory, formal epistemology and welfare economics, and the relationship between these areas.
Notes
[1] Indeed, I’ve changed the names of the women I interviewed, as they did not feel that they can express their views openly.



































































































Connect with us
Facebook
Twitter
Youtube
Flickr