Philosopher Richard Pettigrew (University of Bristol) shares his personal thoughts on changing selves and reflects on our latest Philosophy Live event ‘Dementia and decision-making: How should we make decisions with – or on behalf of – those with dementia?’
Ten years ago, I was trying to decide whether or not to adopt a child and become a parent. I attended information sessions and filled out forms, but I was struggling with the decision whether or not to proceed. What I found difficult was that, for many people and so possibly for me, becoming a parent is what Laurie Paul calls a transformative experience. For these people, becoming a parent teaches them something important about what it’s like to be a parent—or, more precisely, what it’s like for them to be a parent—that they could not have known in any other way; and it also changes some of their desires and wants and preferences and values. It was the second possibility here that really bamboozled my thinking about the decision. At the time, there were various things about the prospect of parenting an adopted child that I valued enormously. Some were moral values: to provide safety and security for someone who needed it. Others weren’t: I valued the prospective pleasure of seeing someone grow up and develop their character, and be there to enjoy that with them along the way. But there were other things I didn’t value about the prospect of parenting. The usual things: loss of the sort of independence I enjoyed at the time; less time to spend with friends and on the sorts of activities outside work I like to do, of which more below. On balance, after weighing up all of these different considerations, I think I valued remaining child-free more than becoming a parent. But I also knew there was a decent chance that would change if I were to become a parent. It was unlikely I’d suddenly place no value on independence and no value on evenings spent with friends, but the weighting I’d give to those things versus the other things I’d gain through parenting would likely shift, and as a result I’d come to prefer being a parent. But how, then, should I make the choice? Using my current values, or those I would likely come to have if I were to become a parent? Perhaps some compromise between the two? This puzzled me as a person, as it had likely puzzled many people before me; and it puzzled me as someone whose academic research work concerns how we should make decisions, just as it had puzzled Laurie Paul, but also Edna Ullmann-Margalit and Krister Bykvist, who have written about the topic as well. And so I did what all sensible people do when faced with decision paralysis: I wrote a book. It’s called Choosing for Changing Selves.
In the book, I offered a perspective on decision-making inspired to some extent by Derek Parfit’s view of persons. I am a person born in the 1980s and extended through time to the present; and hopefully I will also be extended for a decent amount of time into the future. But that person I am is itself a collective or corporate entity. It is composed of a number of different selves. I am not today the same self I was when I was 17, finishing high school and ready to go off to university, though I am the same person; nor am I the same self I was when I turned 30 a little over a decade ago. When I make a decision, then, I am a member of a collective, and I make my decision on behalf of that collective. I am entrusted with executive power over its choices at this time, but in the past other selves were entrusted with that, and in the future further selves will be. So, I am like the head of an academic department in a UK university, a job that rotates among the various members of the department, each one taking on the responsibility at some point, permitted to give some extra weight to their own preferences and projects, but also beholden to the preferences and projects of the other members of the department.
The central suggestion of Choosing for Changing Selves is that we should approach decision-making on behalf of such a collective in the way that we approach decision-making on behalf of other collectives, such as a nation of people, a community of activists, a parish council, a company board, a family, and so on. And this sort of collective decision-making is exactly what we study in social choice theory, voting theory, and related disciplines. I argued for using a particular approach in social choice theory—a particular way of merging the values of all of selves that make up the person I am, possibly giving different weight to different selves based on a variety of considerations—and I applied that to the problem of choosing for a collective of selves, possibly with rather different values, desires, preferences, and projects.
In the end, I didn’t adopt.
The Philosophy Live Panel
Fast forward a few years and, on Tuesday, I was sitting on a panel for an event at the LSE, organised and chaired by Anna Mahtani, on the topic of dementia and decision-making, with the activist and care-giver Ruth Bright, the campaigner and author Nicci Gerard, and the doctor David Jarrett. And it led me to ask whether this way of approaching choices, this collective view of the persons we are, can help us think about the question of decision-making for people with dementia. What follows are some rather disjointed initial thoughts following the panel.
The first thought is a rather obvious one. The view of persons as collectives whose members are different selves—perhaps with different values, personalities, projects, and beliefs—fits well with some of the things people say they fear about developing dementia, or people who’ve recently been diagnosed say they fear about the coming years. Some say they fear they’ll betray themselves; that they’ll do or say something that conflicts with their core values; or, as Nicci Gerard mentioned in the panel discussion, they fear they might become sufficiently disinhibited that they’ll reveal sides of themselves that they dislike and that they’ve worked hard to suppress throughout their lives. On the collectives view, what you fear is handing over the reins to someone you think won’t share your values, or someone you think isn’t trustworthy or competent or capable. It is akin to handing over to a new head of department whom you think will undo the good work that you’ve done, perhaps sully the reputation of the department you’ve worked to build, etc. But of course it is of greater moment, because it is the life, projects, and reputation of the very person you are over which this new self will have control.
This brings me to the second thought. One of the natural questions about decision-making by, or on behalf of, those with dementia concerns living wills and advanced directives. These documents are typically written by someone who hasn’t been diagnosed with dementia, but who wants to make provision for a future in which they are, or who has been recently diagnosed and is in the very early stages of the condition. They specify what that person would like to happen should they reach a particular stage in the progress of the condition. For instance, they might specify that the person would not wish to be resuscitated. Or they might specify that the person has a particular religious or moral commitment that they wish to be respected, even if they come to say later they don’t care about it or they reverse it—perhaps a vegetarian wants to commit their future self, at a later stage in the progression of their dementia, to remaining vegetarian; perhaps an atheist wants to commit their future self to not receiving religious rites on their deathbed; perhaps you want to leave your estate to your family, and want to bind your future self with dementia to not changing that commitment. Or they might simpy specify the person’s taste in music and food and drink, in the hope that their care-givers can arrange for those tastes to be accommodated. The natural ethical question that arises from these documents is this: Should care-givers follow them when the time comes? Should they do so if the person with dementia has clearly expressed opposite desires? Should they do so if they judge that the person with dementia has opposite desires?
One thing I like about the collectives picture is that, when we conceive of ourselves as it suggests, we are less tempted to think that there is such a thing as the core or real person that a later self might betray or reject or simply get confused about. There is just the sequence of selves, some with conflicting values, and they together make up the person, none more so than another—while we tell ourselves narratives to give our life a shape, and while the lives of some people really do have a natural straightforward development story, many are jumbles of different selves; and, I would say, none the worse for that.
But this raises the question why an earlier self should have dominion over the later self in the way they attempt to have when they write a living will or an advanced directive. If the earlier self, writing the living will, wants to leave their estate to their family, but the later self with reasonably advanced dementia wants to leave it to a charity they’ve recently heard about from talking to a care-giver, why should the earlier self take priority? If you think the later self betrays a core commitment of the person to whom they belong by turning away from their family, perhaps because all of their earlier selves were completely devoted to those people and so reflect what the person truly values, I think it is tempting to say that the later self with dementia has become confused about what they really want and so should be ignored or at least given less weight. But if you see the later self simply as a later member of the collective that also includes those family-focused earlier selves, I think there’s less inclination to say that.
Of course, you may nonetheless think that the earlier selves should have dominion in this case, for the estate is something built up by all of them collectively. This is an interesting case. Often in the philosophical literature on decision-making, people think that the past preferences of the decision-maker shouldn’t count at all. Here’s Richard Brandt:
If a person is deciding what to do for himself, we should think it strange for him to decide on the basis partly of what he wanted or did not want ten years ago. (171, Morality, Utilitarianism, and Rights)
And Parfit thinks it would be strange for him, in his late twenties, to devote all his energies to becoming a poet, even though he doesn’t want that at the time but did want it when he was a younger man.
Yet of course living wills assume exactly the opposite. In fact, in Choosing for Changing Selves, I argued that there are cases in which the preferences of past selves should count, such as when those past selves made substantial sacrifices to benefit their future selves. Perhaps we can understand the case of the changed will in this way: the later self, whether with dementia or not, is beholden at least partly to the preferences of the earlier selves because they made the sacrifices to build the estate that is there to be bequeathed. But that’s less plausible in the case of the lifelong atheist who goes against their living will to request a priest on their deathbed, or the vegetarian who goes against their living will to request a more omnivorous diet in the future. In those cases, it’s harder to see that the earlier selves have made a sacrifice that leaves the later self obliged to defer to the earlier selves’ desires and projects. Perhaps we might say that the atheist has sacrificed a certain comfort of mind by not living with the balm of religious belief; and that the vegetarian has sacrificed a certain amount of pleasure in order to ensure a moral life; and in both cases the later self wants to disregard those sacrifices. But even if we do say that, it’s not so obvious that these sacrifices create obligations for the later self. Not all sacrifices do. I suppose many will think that no sacrifices that one individual makes can create obligations in another if the other didn’t ask for them. But it does seem that the obligation to pay your taxes, for instance, is born of others paying theirs, sacrificing some of their wealth to support the communal infrastructure and services, and that obligation arises even if you didn’t ask the others to pay their taxes. So our question might become: under what circumstances does a sacrifice by one create an obligation in another who benefits from the sacrifice? A tricky question.
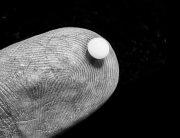
But many think that this is irrelevant: living wills and advanced directives should be respected regardless of how the calculus of sacrifice and obligation plays out. In those cases, if the living will is to have any authority, we must say that the preferences of the later self with dementia can somehow be ignored or overridden. Why might that be? Something that decision theory does well is to pick apart the components that go into determining our preferences. According to the standard story, our preferences are determined both by our beliefs, which say how the world is, and our desires, which say how much we value different ways the world might be. So if I want to leave money to charity, that will be based partly on my beliefs about what effects doing that might have, and partly on how much I value the different possible effects. It is plausible that, as dementia advances, our beliefs about what effects different possible options will have become less reliable—our understanding of how things go in the world can become more fragmented and we might find reasoning through the consequences more difficult. And I think this is often why people say that someone with more advanced dementia should be entrusted with fewer decisions about their well-being. But, while it might be true that the belief component of their preferences is less reliable, I think it’s less plausible that the desires they have—the values they assign to different ways the world might be—are less legitimate. And so, while it might be legitimate to support someone with dementia to help them make a good decision by filling in the gaps in their knowledge of what consequences different options are likely to have, we should be very slow to impose values that are not the ones they espouse.
An analogy is helpful here, I think. Unlike my three co-panellists, I don’t have much experience working with people with dementia. But I do have a lot of experience working with adults who’ve had cognitive disabilities throughout their lives. For the past twenty years, I’ve helped to run a disabled club for adults with cognitive and learning disabilities. It meets one evening per week for two hours, and we organise all sorts of activities, from dance and movement evenings to game shows. Throughout the panel on Tuesday, I was struck by how much we might learn by thinking of someone who has more advanced dementia in the way we think of some of the people I work with at the evening club. In those latter cases, as a care-giver, you are rarely tempted to think that the person’s wants and values are illegitimate or apt to be ignored. Rather, you just think that someone with a certain sort of cognitive disability might be less able to understand the consequences of different choices they might make, and so less able to identify the best means to their ends. And so you support them to identify those means, but you aren’t tempted to impose different ends on them.
This leads me to the final thought coming out of Tuesday’s panel. People often seem tempted to treat people with dementia as beholden to their earlier selves’ desires because they think of them as ‘diminished’ versions of those earlier selves, rather than as different selves with different competences—the description came up a couple of times in the panel, and Ruth Bright gave a powerful account of why we should move away from that framing. By attending to the trajectory of the life, viewing the later self only by comparison with the earlier selves and noting the ways in which they are unable to do certain things the earlier self could do, they fail to treat the later self as fully an individual whose ends are legitimate, but who might have trouble identifying the best means to their ends. Again, attending to the analogy with people who have had some of these cognitive disabilities throughout their lives is illuminating. For in those cases there is no earlier self without the disability against which to measure the later self. You are more inclined to see them as fully individual.
This points to an interesting parallel with adaptive preferences. One reason people sometimes dismiss the desires of a person with dementia as illegitimate or confused is that they view those desires as much smaller or more limited than the ones they take to be befitting of that person. “This person was once a successful lawyer, you know, taking pleasure in fine foods and good books and holidays in beautiful cities and trips to great art galleries. Now they seem to value nothing more than sitting colouring in a picture or dancing with other people in their residential unit to music from a stereo. How could you view them as anything other than diminished? They have surely merely adapted their preferences to the vastly reduced range of options that their condition leaves open to them.” Such is a thought one hears reasonably often. And from it follows that the preferences so adapted are not really legitimate ones, and so might be ignored, if necessary.
But I think this is a case in which we shouldn’t be so quick to dismiss adaptive preferences. For one way in which they might be formed is quite virtuous. When your options are limited, you give greater attention to the details of those available to you. It is a commonplace to say that, in their hurried lives, the successful lawyer rarely pays proper attention to the joys that quite ordinary aspects of everyday life afford: the cliché is the beauty of the nature around them or the kindness of the people with whom they interact, but there are many other features as well, and certain activities that many look down upon hold innumerable joys to which one better attends when that activity is one of the few available to you. So, while adaptive preferences formed under the weight of oppression might well be problematic, it is much less clear that the same is true of those developed because the person attends better to the genuinely valuable features of an activity when it is one of the few available to them. It’s possible that this goes some way to explaining of the phenomenon we often see that, following a diagnosis of a serious medical condition, a person’s well-being report plummets, but soon rebounds back to original levels.
All of this is not to say, of course, that dementia is not a condition that can cause great suffering, nor that we are necessarily wrong to fear it. The confusion that results can be very distressing; the loss of capacities and memories one very much valued can be devastating; and there is the possibility that the ways in which one related to friends, family, and other loved ones may no longer be possible because your once shared stock of stories is unavailable to you and you find sustained conversation much harder and quite confusing. This can be a terrible disease. But we should hesitate to dismiss the preferences of those who have it just because they differ from those they had before. We should not necessarily view them as the corrupted preferences of an enduring person, but the new preferences of a self that belongs just as much to that person as their earlier selves did.
By Richard Pettigrew
Richard Pettigrew is a Professor in the Department of Philosophy at the University of Bristol.
Credits
This blog article has been posted on Richard Pettigrew’s substack and Richard has kindly allowed us to cross post it here as well.
The recording of the Philosophy Live panel ‘Dementia and decision-making’ is available on the LSE YouTube channel.



































































































Connect with us
Facebook
Twitter
Youtube
Flickr